Outcome of Epidemiological Surveillance of Bacterial Meningitis in Mali from 1996 to 2016: What Lesson to Learn?
Souleymane C, Abdelaye K, Ibrehima G, Abdou M, Kadiatou D, Oumou CY, Aly L, Seydou D and Flabou B
Souleymane C1, Abdelaye K1, Ibrehima G1,2, Abdou M1, Kadiatou D1, Oumou CY3, Aly L1, Seydou D1 and Flabou B1,2
1National Institute for Research in Public Health (INRSP), Bamako, Mali
2Faculty of Pharmacy, University of Sciences, Technics and Technology of Bamako, Mali
3Epidemiological Surveillance, Unit of the National Direction for Health (DNS), Mali
- *Corresponding Author:
- Souleymane C
National Institute for Research in Public Health (INRSP)
Bamako, Mali
Tel: +22320214231
Fax: +22320210642
E-mail: sbcoulibaly1@yahoo.fr
Received date: August 12, 2017; Accepted date: September 07, 2017; Published date: September 09, 2017
Citation: Souleymane C, Abdelaye K, Ibrehima G, et al. Outcome of epidemiological surveillance of bacterial meningitis in Mali from 1996 to 2016: what lesson to learn? J Mol Pathol Epidemiol. 2017;2:02.
Copyright: © 2017 Souleymane C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Bacterial meningitis remains a public health problem in Mali. The aim of this work is to describe epidemiological outcome of meningitis surveillance.
Methods: It is a retrospective study of meningitis data from 1996 to 2016 at the National Institute for Public Health Research (INRSP) in Mali.
Results: A total of 12556 cases were diagnosed at the INRSP against 36065 notifications at the National Direction for Health. We had 3306 positive cases and recorded 3158 deaths. Prevalence decreased from 0.078% in 1996 to 0.004% in 2016. The majority was male with 59.90%. Neisseria meningitidis represented 43.77% of the germs, followed by Streptococcus pneumoniae (31.40%) and Haemophilus influenzae (23.44%). The most affected age group was 0-14 years, i.e. 86.63%.
Conclusion: These results show the dynamism of epidemiological monitoring in Mali. A-conjugate vaccine may be an alternative to Mali because NmA has almost disappeared. We believe that the use of vaccines would prevent significant endemic morbidity rate and many deaths due to meningitis.
Keywords
Epidemiological; Surveillance; Meningitis; Mali
Introduction
Bacterial meningitis is defined as acute or chronic inflammation of the mining and subarachnoid spaces due to the development in the organism of a generally saprophytic endocellular bacterium of the human nasopharynx. Meningitis is an acute infection of the protective membrane covering the brain and spinal usually caused by encapsulated bacteria such as Neisseria meningitidis, Haemophilus influenzae or Streptococcus pneumoniae. It is an infectious and contagious disease that responsible of death or severe neurological squeal if untreated [1]. In the intertropical zone of Africa and probably in all the countries of the Third World, purulent meningitis remains worrying because of their frequency and severity [2]. Mali, as other countries in the African meningitis belt, is an area with repeated epidemics of meningococcal meningitis. It is a significant cause of death.
In Mali, huge progress has been made in monitoring meningitis since the 2001-2002 epidemiological period regarding the implementation of the Integrated Disease Surveillance and Response (IDSR), the adoption and implementation of Standard Operating Procedures (SOPs) for enhanced meningitis surveillance [1] the moving to case-by-case surveillance (CCS) of meningitis [3]. Despite to these actions undertaken, we registered each year some cases often accompanied to epidemic risk. During the surveillance reinforced of the meningitis the sporadic cases were recorded of way disperses in the time and in the space often provoking localized epidemics (2008). The last epidemic of meningococcal meningitis in Mali took place in 2016 in one district (Ouelessebougou) situated at 80 kilometer to Bamako. According to national direction of health, a total of 741 suspected cases of meningitis including 16 deaths were reported in Mali in 2016.
There is a risk of passage of the epidemics of a country to another. The burden of disease and deaths evaluation due to bacterial meningitis may suggest priorities in the current use of available vaccines and help in the evaluation of new vaccines against the three major etiologic agents: Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae b [2]. The aim of this retrospective work in Mali is to describe the outcome of 21 years’ surveillance in the view to show lesson to learn.
Surveillance and Methods
The epidemiological surveillance is led since the peripheral level with the Centers of Communal Health and the Centers of Reference Health by the detection, the notification, the collection of the samples, the preliminary analysis (cool state, Gram) and the transportation of the samples to the intermediate level (provincial) accompanied of the card of individual notification of case. The region through the laboratory of the provincial hospital analyzes the samples so possible; the provincial direction of health is assigned to make the conditioning and transportation of the samples to the level central to the section epidemiological surveillance of the national direction of health. The national direction of health routes the samples to the National Institute for Research in Public Health (INRSP) for confirmation by the culture and/or the PCR. Otherwise the townships (Communes) of Bamako and the Centers Health of Reference no far from Bamako bring their samples directly to the INRSP.
Type and period of study
The loaded surveillance of the provincial directions of health notify daily by telephone and daily by electronic mail to the section epidemiological surveillance of the national direction of health the epidemiological situation of the province. This notification includes the notified cases appropriated and of the notified cases none appropriated. The labline (results of the laboratory) is transmitted daily to the national direction of health by the INRSP. The old-fashioned information is made according to the sanitary pyramid of Mali: national level, provincial level and peripheral level.
Specimen and data collection system
The Cerebrospinal fluid (CSF) is collected at the suspected cases in the sanitary establishments, the centers of communal health, the centers of reference health, the hospitals and the private structures accompanied by card of individual notification of case.
Data collection included all weekly notifications of suspected cases of meningitis at the Unit of Epidemiological surveillance (SSE) of the National Direction for Health (DNS), cerebrospinal fluid (CSF) samples sent to the INRSP, and analytical results of these. Suspected cases were enrolled according to the WHO case definition [1,3]. Data were collected from the laboratory registers and databases, individual case reports, the SSE/DNS database during the study period. For each case, our recorded information was based on the demographic characteristics and results of the LCR analysis (cell count, Gram staining, latex, culture and PCR). The PCR data were only available from 2008, the starting date of the classic PCR and since 2012 we have been using real time PCR. We also examined the basis of the weekly notification of SSE/DNS notification diseases (MADO) for suspected cases of meningitis and lethality. A case of bacterial meningitis was said to be confirmed if at least one of the three
Data analysis tests is positive (soluble antigen, culture, PCR). The data were processed and analyzed using Excel and Epi info 3.5.4.
Results
Surveillance bacterial meningitis
The epidemiological surveillance of meningitis between 1996 and 2016 recorded 36065 cases, 3158 deaths with a lethality of 8.75% in Mali. The average annual notification was 1717 cases with a maximum of 11228 cases in 1997 and a minimum of 342 cases in 2009. The average case lethality was 6%, the maximum 11% (1996, 1998, 1999, 2000 and 2001) and the Minimum 1 (2012) (Table 1). The prevalence of meningitis ranged from 0.078% in 1996 to 0.004% in 2016. During the period 12556 LCR was collected, sent and analyzed at INRSP against 36065 notifications at DNS or 34.81% rate of LCR sample of which 3306 positive; a positivity of 26.33% (Tables 1 and 2). The District of Bamako predominated with 53.20% of the samples, followed by Koulikoro with 25.10%. The sex ratio was 1.5 in favor of the male sex, or 59.9% of the cases. The sampling was adequate at 89%, turbidity at 10.20% and the case majority was recorded during April and March respectively 16.70% and 16.20%.
| Year | Suspected Cases notified | Death | lethality rate | CSF taken |
|---|---|---|---|---|
| 1996 | 7413 | 852 | 11 | 488 |
| 1997 | 11228 | 1126 | 10 | 205 |
| 1998 | 2712 | 288 | 11 | 467 |
| 1999 | 1038 | 118 | 11 | 1063 |
| 2000 | 862 | 93 | 11 | 905 |
| 2001 | 1116 | 127 | 11 | 969 |
| 2002 | 787 | 61 | 8 | 287 |
| 2003 | 1147 | 73 | 6 | 587 |
| 2004 | 1476 | 57 | 4 | 1457 |
| 2005 | 454 | 23 | 5 | 577 |
| 2006 | 1039 | 75 | 7 | 482 |
| 2007 | 978 | 48 | 5 | 514 |
| 2008 | 1538 | 85 | 6 | 816 |
| 2009 | 342 | 30 | 9 | 287 |
| 2010 | 485 | 34 | 7 | 471 |
| 2011 | 512 | 17 | 3 | 447 |
| 2012 | 900 | 12 | 1 | 565 |
| 2013 | 361 | 9 | 2 | 420 |
| 2014 | 400 | 6 | 2 | 355 |
| 2015 | 536 | 8 | 2 | 504 |
| 2016 | 741 | 16 | 2 | 690 |
| Total | 36065 | 3158 | 8,75 | 12556 |
| CSF: Cerebrospinal fluid | ||||
Table 1: Distribution of the cases of meningitis, death, lethality rate and CSF of 1996-2016 in Mali.
Etiology of bacterial meningitis in Mali
The laboratory result with 43.77% (1447/3306) of Neisseria meningitidis, 31.40% (1038/3306) of Streptococcus pneumoniae, 23.44% (775/3306) of Haemophilus influenzae and 1.39% (46/3306) from other germs as reflected (Table 2).
| Year | Germs | Total | |||
|---|---|---|---|---|---|
| Nm | Spn | Hi | Others | ||
| 1996* | 422 | 29 | 26 | 0 | 477 |
| 1997* | 104 | 11 | 11 | 0 | 126 |
| 1998* | 127 | 51 | 43 | 1 | 222 |
| 1999 | 17 | 80 | 78 | 5 | 180 |
| 2000 | 2 | 87 | 78 | 0 | 167 |
| 2001 | 17 | 47 | 69 | 0 | 133 |
| 2002 | 38 | 173 | 135 | 0 | 346 |
| 2003 | 74 | 133 | 104 | 0 | 311 |
| 2004 | 25 | 64 | 76 | 6 | 171 |
| 2005 | 8 | 22 | 19 | 2 | 51 |
| 2006 | 36 | 22 | 15 | 7 | 80 |
| 2007 | 67 | 18 | 6 | 0 | 91 |
| 2008* | 153 | 33 | 20 | 2 | 208 |
| 2009 | 36 | 2 | 3 | 1 | 42 |
| 2010** | 35 | 12 | 1 | 3 | 51 |
| 2011*** | 50 | 10 | 5 | 1 | 66 |
| 2012 | 145 | 34 | 7 | 7 | 193 |
| 2013 | 7 | 26 | 21 | 1 | 55 |
| 2014 | 14 | 62 | 13 | 2 | 91 |
| 2015 | 25 | 39 | 10 | 1 | 75 |
| 2016 | 45 | 83 | 35 | 7 | 170 |
| Total | 1447 | 1038 | 775 | 46 | 3306 |
| *Epidemic years **Introduction de MenAfriVac(Meningococcal A Conjugate Vaccine for Africa) ***Campagne de masse avec le MenAfriVac(Meningococcal A Conjugate Vaccine for Africa) Nm: Neisseria meningitidis, Spn: Streptococcus pneumoniae, Hi: Haemophilusinfluenzae. Others: Streptococcus agalactiae, Salmonella spp, Escherichia coli, Klebsiellaspp, Acinetobacterspp, Citrobacterspp, Klebsiellapneumoniae, Enterobacterspp, Cryptococcus neoformans, Candida albicans |
|||||
Table 2: Distribution of the germs identified in the CSF of 1996 - 2016 in Mali.
Meningococcus evolution in Mali
Neisseria meningitidis A caused several epidemics in Mali (1996, 1997, 1998, and 2008) before the introduction of A - conjugate vaccine "MenAfriVac" in 2010. In addition, NmC caused the last epidemics in Mali in 2016.
Among the meningococcus identified between 1996 and 2016, NmA was predominant with 76.36%, followed by NmW135 (17.62%), NmX (3.45%), NmC (1.73%) and NmY, 21%).
Neisseria meningitidis A predominated until the introduction of the "MenAfriVac" in 2010, followed by NmW135 which peaked in 2012 (Figure 1).
Figure 1: Evolution of the meningococcal meningitis from 1996-2016 in Mali. NmA: Neisseria meningitidis serogroup A, NmW135: Neisseria meningitidis serogroup W135, NmC: Neisseria meningitidis serogroup C, NmY: Neisseria meningitidis serogroup Y, NmX: Neisseria meningitidis serogroup X, Nm: Neisseria meningitidis no serogroup.
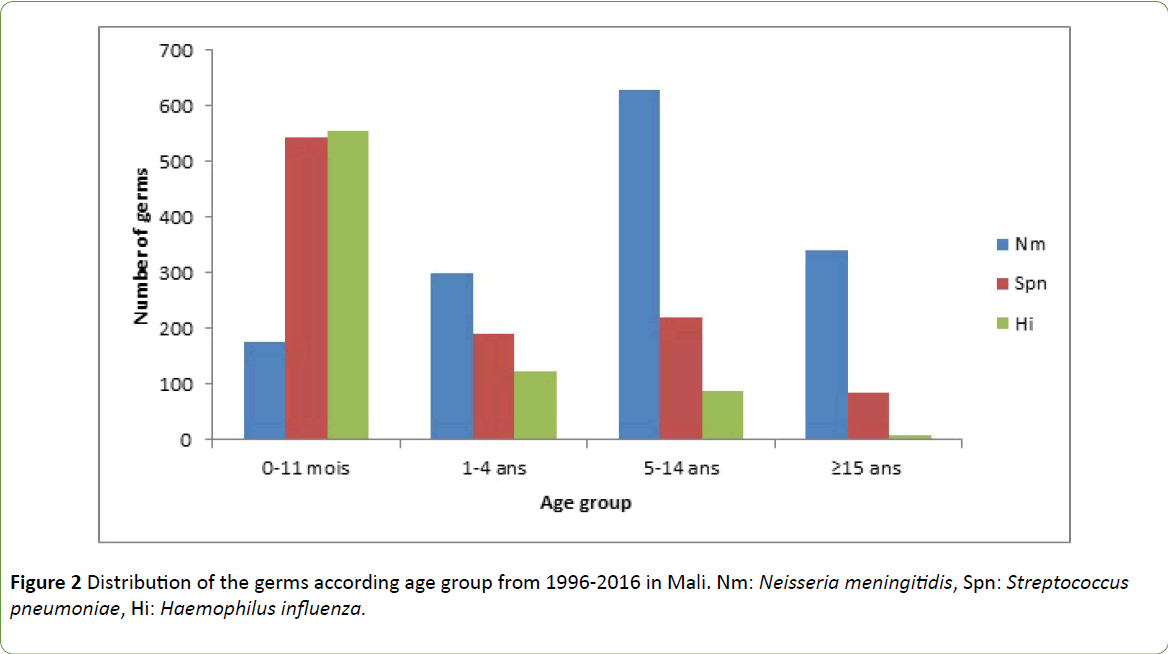
Risk group
The age group most affected by meningitis was 0-14 years, i.e. 86.63% by the 3 germs combined (Nm, Spn and Hi). Haemophilus influenzae and Streptococcus pneumoniae are predominant in the 0-11 month ages ranging with 71.48% and 52.41%, respectively; Neisseria meningitidis for the 1 to 4 year age groups, 5 to 14 years and 15 years and over, respectively, 48.94%; 67.20% and 78.44%. The average age was 9.03 with a minimum of less than one day and a maximum of 97 years. The median was 4 and the mode was equal to 1 (Figure 2).
Discussion
This retrospective study of meningitis surveillance data over a two-decade period showed the extent of bacterial meningitis in Mali, the importance and place of meningococcus among the agents causing bacterial meningitis. Among the suspected cases of meningitis (36065 cases), 34.81% received a cerebral spinal fluid (CSF) sample (12556). This highlights effort to be made in case-by-case surveillance. Study performed by Cadoz et al. in Dakar over 10 years, there were 3422 cases of purulent meningitis [4]. According to the report from World Health Organization in 1999, Niger recorded 7078 cases of bacterial meningitis diagnosed in the laboratory over a period of 15 years. 2 Mali, like other countries in the meningitis belt, was under increased meningitis surveillance until 2010 [5].
Following the introduction of the "MenAfriVac" conjugate A vaccine in the three countries (Burkina Faso, Mali and Niger) in 2010-2011, case-by-case surveillance (SCC) was introduced where each case must be Lumbar puncture and laboratory confirmation [3]. The average lethality was 6%, the high lethalities were recorded between 1996 and 2001, going up to 11 and the lowest was 1 in 2012. According to Campagne et al in Niger the annual incidence of bacterial meningitis is between 27.3 and 347.6 (average: 101) per 100,000 inhabitants and the death rate between 6.0 and 27 (average: 17) per 100,000 inhabitants [2]. The prevalence of bacterial meningitis in Mali has decreased in recent years from 0.078% in 1996 to 0.004% in 2016. This decline in meningitis can be explained by the introduction of A-conjugated vaccine in 2010 [6]. According to Nicolas' study in 2012 the prevalence of meningococcal carriage in Africa varies from 3 to 27%, several studies give an average prevalence of 6-8% [7]. Out of a total of 12556 LCR samples taken, 3306 were positive, i.e. a positivity of 26.33% during the study period.
The District of Bamako, the capital city of Mali, predominated with 53.20% of sampling, followed by Koulikoro with 25.10%. These two regions have an easy access to the reference laboratory, which could explain their rate, but also the presence of third level hospitals and the concentration of the population of the capital city and its surroundings. The study by Guindo et al made the same observation that Bamako had recorded 68.5% of LCR between 2005-2007 in Mali [8]. Male to female ratio was 1.59, i.e. 59.9%, is comparable to the result of Kenza in 2010 in Marrakech, which found a male predominance to 64% (Wright 2010, personal communication). Samples were adequate at 89% and disorders at 10.20%. These data differ from those obtained by Guindo in 2013 in Mali, ie 58.65% of suitability and 14.42% LCR turbidity (Wright 2013, personal communication) and Kenza in Marrakech in 2010 with 83% cloudy CSF. The majority of cases were recorded in April and March respectively 16.70% and 16.20%. The meningitis predominance is observed during this period, as it is favored by high heat and harmattan. This has already been done by studies that have interested other countries in Africa, including Niger [9] Tchad [10] Burkina Faso and the African meningitis belt [11].
The majority of meningitis (43.77%) was due to Neisseria meningitidis, followed by Streptococcus pneumoniae (31.40%) and Haemophilus influenzae (23.44%). On the other hand, in the Kenza study, the main germ was Streptococcus pneumoniae (48.71%), followed by Neisseria meningitidis (32.05%) and Haemophilus influenzae type b (19.23%) [10] (Kenza, 2010). Despite the introduction in the routine Expanded Programme for Immunization (EPI) in Mali, vaccines against Haemophilus influenzae type b in 2005 and pneumococcus in 2011, we are still seeing their high incidence in pediatric meningitis. The pneumococcal vaccine (Prevnar 13®) covers only 13/92 known serotypes (Wright 2015, personal communication).
Among identified groups of Haemophilus influenzae; 73.53% was Haemophilus influenzae type b (Hib) and 26.47% non b. NmA was predominant in meningococcal disease with 76.36%; followed by NmW135 (17.62%), NmX (3.45%), NmC (1.73%) and NmY (0.21%). NmA has been causing several epidemics in Mali (1996, 1997, 1998 and 2008) and in the countries of the African meningitis belt. It was still present in non-epidemic years until the introduction of A-conjugate vaccine in 2010. Only one case of NmA was identified in Mali in the health district of Keniéba, region of Kayes in 2016. It emerges after investigation that the child was not vaccinated. Since 2010, the gradual introduction of "MenAfriVac" into the epidemic-prone areas of the 26 countries of the African meningitis belt has led to a dramatic decline in the number of cases of NmA meningitis and the elimination of NmA epidemics. At the same time, the relative proportion of cases due to other serogroups (W, X and C) and Streptococcus pneumoniae (Spn) increased [12,13].
In the 0-11 month-age group, Haemophilus influenzae (71.48%) and Streptococcus pneumoniae (52.41%) were the most frequent germs, but Neisseria meningitidis was also present at 13.75%. Neisseria meningitidis was the most common in the 1-4 years age group, 5-14 years and 15 years and older, with 48.94%; 67.20% and 78.44% respectively. Overall, the group most affected by meningitis was 0-14 years i.e. 86.63% by the 3 germs combined (Nm, Spn and Hi). Our results have been confirmed by other studies in Africa and around the world. The study of Guindo in 2013 in Mali, [8] Kenza in 2010 in Morocco(Wright 2010, personal communication), Campagne in 1999 in Niger,[2] Isabelle in 2012 in France, [14] and that of Jessica in 2015 in the United States [15].
Conclusion
These results show the dynamics of the epidemiological surveillance in Mali in all its components with a major observation, the reduction of epidemics on a large scale substituted by sporadic or endemic forms at the pediatric level. The introduction of A-conjugate vaccine could be a solution to Mali because NmA has almost disappeared but replaced by other serogroups including NmW135, NmC and NmX. We believe that the use of vaccines against S. pneumoniae and Hib under the Expanded Program for Immunization (EPI) would prevent significant endemic morbidity and many deaths due to meningitis. However, it would be necessary to improve some points:
Control of emerging meningococcal serogroups.
Case-by-case surveillance at all levels of the health pyramid.
The number of serotypes covered by vaccines.
References
- World Health Organization / Center for Diseases Control and prevention (2010) Technical guide for surveillance integrated of the diseases and the riposte in region African. Geneva: World Health Organization.
- Campagne G, Schuchat A, Djibo S, Ousseini A, Cisse L, et al. (1999) Epidemiology of bacterial meningitis in Niamey, Niger, 1981-96. Bull World Health Organ 77: 499-508.
- Ministry of Health/ World Health Organization/Center for Diseases Control and prevention (2010) National guide of surveillance case by case of the bacterial meningitis, Mali.
- Cadoz M, Denis F, Mar ID (1981) Epidemiological survey of the cases of purulent meningitis hospitalizes in Dakar during the decade 1970-1979. Bull World Health Organ 59: 575-584.
- World Health Organization (2008) Procedures operational standards for the surveillance reinforced of the meningitis in Africa. Geneva: World Health Organization.
- World Health Organization (2014) Guideline meningitis outbreak response in sub-Saharan Africa, Press WHO, Geneva.
- Nicolas P (2012) Meningococcal meningococcal epidemics in the meningitis belt (1995-2011) and introduction of meningococcal conjugate vaccine.Med Trop 22: 246-258.
- GuindoI, Coulibaly A, Dao S, Traoré S, Diarra S, et al. (2011)
Clones of strains of Neisseria meningitidis in Mali. Med Mal Infect. 41: 7-13. - Juliette P (2012) Spatial epidemiology of the meningitis to Meningococcus in Niger - influence of the climatic, epidemiological factors and socio-demographics on the dynamic spatio-temporal of the epidemics.
- Garcia V, Morel B, Wadack MA, Banguio M, Moulia-Pelat JP, et al. (2004) Epidemic outbreaks of meningitis in the Department of Western Logone (Chad): study descriptive data from the Ministry of health care from 1998 to 2001. Bull SocPatholExot 97:183-188.
- World Health Organization. Guide struggle against the epidemics of meningitis to Meningococcus. Geneva: World Health Organization; 1998.
- World Health Organization (2015) Meningitis to Meningococcus memorandum.
- World Health Organization (2016) Weekly epidemiological record. 91, 209-16.
- Isabelle P. Epidemiology of acute meningitis in France 2012.
- MacNeil JR, Bennett N, Farley MM, Harrison LH, Lynfield R, et al. (2015) Epidemiology of infant meningococcal disease in the United States, 2006-2012. Pediatrics 135: e305-11.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences